- For FIGHT patients who have any sick symptoms or have been exposed to mpox: Call your Philadelphia FIGHT health center and ask to speak to a nurse.
- During the month of August, mPox vaccines are offered for existing patients at the John Bell Health Center, 1207 Chestnut Street, 3rd Floor. For more information, please call 267-725-0252.
- IMPORTANT: the CDC suggests some patients should wait 4 weeks after getting the mpox vaccine to get a COVID-19 vaccine.
- You may also get mpox vaccines from our colleagues at Bebashi and Mazzoni, as well as Philadelphia Rite Aid locations. Note: Rite Aid may charge to administer the vaccine depending on your insurance.
Mpox Health Information
On December 7, 2022 the Philadelphia Department of Public Health – following CDC guidance – announced that mpox vaccine providers may now optionally give the vaccine intradermally (a bubble under the skin) or subcutaneously (a small needle injection). FIGHT may still default to intradermal injections to save supply of the vaccine, but any patient may request a subcutaneous shot – this is a good option if you had a strong reaction at the site of your first intradermal injection.
On November 28, 2022 The World Health Organization (WHO) renamed ‘monkeypox’ to ‘mpox’ – and the US Department of Health and Human Services agreed it will use the new name going forward “to avoid stigma around the disease and further promote access to quality care
On June 2, 2022, the Philadelphia Department of Public Health announced the first case of MPox Philadelphia. On July 23, the World Health Organization declared Mpox a “public health emergency of international concern.” Our goal is to provide information about monkeypox without contributing to stigma. Mpox can affect anyone, regardless of gender identity or sexual orientation.
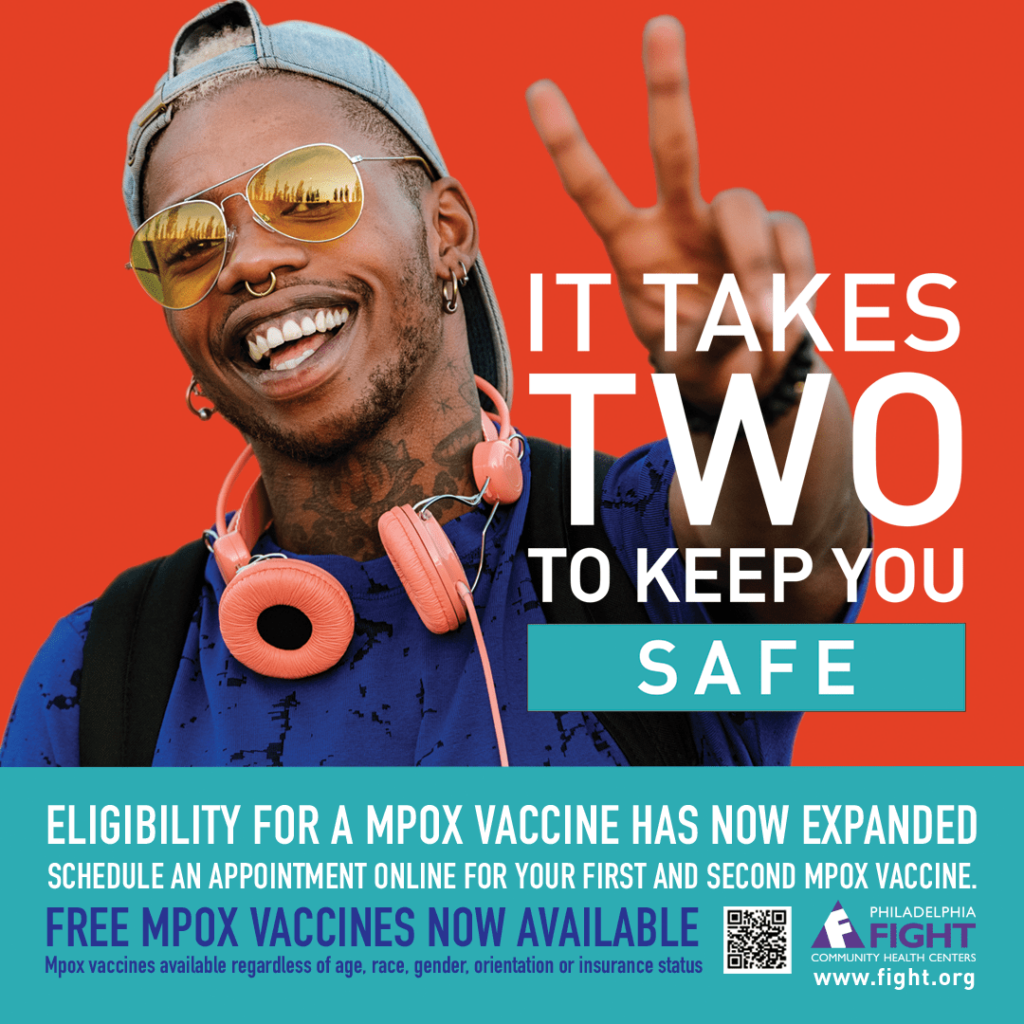
Mpox Vaccine Eligibility
Mpox vaccine availability has greatly improved: Anyone who feels they are at risk for acquiring monkeypox is now eligible for vaccination.
If you received your first dose already, get your second dose.
FIGHT outreach will continue to those who are most at risk, including gay, bisexual, transgender, other men who have sex with men, or non-binary persons who meet the following criteria:
- Have had multiple or anonymous sex partners in the past 14 days.
- Have had any newly diagnosed STI in the past 12 months, including gonorrhea, chlamydia, early syphilis, or HIV.
- Have recently attended or plan to attend any venue where anonymous sex or sex with multiple partners will occur (e.g. saunas, bathhouse, sex clubs, sex parties).
- Have met recent partners or plan to meet new partners through social media platforms (such as Grindr, Tinder or Scruff), or at clubs, raves, sex parties, saunas).
In addition, anyone with known close contact (skin-to-skin) with someone with Mpox in the past 14 days should be vaccinated immediately.
Recording of FIGHT’s Community Conversation on Monkeypox
This video is a recording of Philadelphia FIGHT and JD Evans Solutions’ Community Conversation on Monkeypox, held on Wednesday, August 3, 2022. Please note, there are images in this recording that are graphic in nature and shared for the sole purpose of public health education.
FAQ
Frequently Asked Questions
The best way to avoid getting mpox is to avoid close, skin-to-skin contact with people of unknown health status or who actively have mpox. You may choose to limit physical intimacy with sexual partners whose health status and recent travel history are unknown to you. We understand this is not possible for everyone. You may also choose to ask new sexual partners about whether they have any of the early symptoms of mpox, such as fevers, swollen glands, body aches, or a rash. Try to avoid contact with any bumps or blisters on a person’s skin or near their genitals and anus, if possible.
If you know someone with mpox, avoid close, prolonged, physical contact and touching things they have touched. Wash your hands frequently with soap and water and use hand sanitizer.
Mpox is often spread through:
- Close, personal, skin-to-skin contact
- Direct contact with mpox rash, sores, or scabs
- Oral, anal, and vaginal sex
- Hugging, massage, and mutual masturbation
- Dancing and clubbing with prolonged skin-to-skin contact
Mpox can also sometimes spread by:
- Contact with objects, fabrics (clothing, bedding, or towels), and surfaces that have been used by someone with mpox
- Through respiratory droplets or oral fluids from a person with mpox
People with mpox are most contagious and can infect other people while they have a rash with bumps and blisters. It is possible someone is contagious before a rash develops. A person is contagious until after all the blisters have scabbed over, fallen off, and new skin has grown back. This usually takes 2-4 weeks after the rash first develops. People with a mpox rash should avoid close, skin-to-skin contact with people. People with mpox should avoid sharing bedding, towels, clothes, sex toys, and other objects until their rash is healed.
Symptoms usually start a week or two after exposure to someone with mpox. It sometimes starts with symptoms that might feel like the flu—fever, headache, body and backache, swollen lymph nodes, and chills—but some people do not experience these flu-like symptoms, at all. In the weeks after exposure, a rash resembling bumps or blisters develops. The rash can be seen anywhere on the body including the face, mouth, hands, genitals, or anus. This rash can last up to two to four weeks.
Our biggest concern with mpox is that it will spread among vulnerable communities with little access to and/or trust in the public health system. To date, about 96% of all mpox cases in the United States have been among men who have sex with men. These men have a median age of 36. For people living with undetectable and well-managed HIV, it seems unlikely that mpox will cause more severe disease than it does in people not living with HIV. For people who engage in in-person sex work and survival sex, there is increased concern, as mpox is easily spread by close, skin-to-skin contact.
Lesions, headaches, debilitating pain: Gay men with mpox share their stories | July 6
Mpox is a disease caused by a virus that is usually found in Central and West Africa. Monkeypox was first discovered in laboratory monkeys in 1958. Monkeypox was reported in humans for the first time in 1970. It is called monkeypox because the disease was first discovered in monkeys. The World Health Organization is working to change the name of the disease to make it less stigmatizing.
If you are a Philadelphia FIGHT Community Health Centers patient and are experiencing symptoms consistent with mpox or think you were exposed to mpox, please call your health center and ask to speak to a nurse. Please do not come into the clinic before speaking to a nurse on the phone. If you are not a Philadelphia FIGHT Community Health Centers patient, please contact your healthcare provider and check the Philadelphia Department of Public Health website for information and resources.
In May 2022, about 200 cases of mpox were reported in Europe, North America, Israel, and Australia. Since then, more cases have been identified around the world, including in Philadelphia and Pennsylvania. No one is known to have died in the current outbreak.
To date, 96% of all cases in the United States have been among men who have sex with men. Itis critical to note that mpox can affect anyone, regardless of gender identity or sexual orientation, and despite a recent increase in cases, it is still considered a very rare infection Widespread transmission is currently considered very unlikely. Nevertheless, there is widespread concern among the LGBTQIA+ community both globally and here in Philadelphia, focused on the ways the community can educate and protect itself.
Local News
- Philly’s LGBTQ network has rushed to offer mpox information and services amid slow public health response | July 26, 2022
https://www.inquirer.com/health/monkeypox-philadelphia-vaccine-information-lgbtq-stigma-20220726.html
- Are you at risk of getting mpox? Here’s everything you need to know | July 25, 2022
https://www.inquirer.com/health/monkeypox-outbreak-2022-philadelphia-cases-spread-vaccine-prevention-20220725.html - Health Department to Expand Monkeypox Vaccine Administration | July 19, 2022
https://www.phila.gov/2022-07-19-health-department-to-expand-monkeypox-vaccine-administration/ - Philadelphia’s mpox vaccine supply is getting a big boost, allowing more people to get the shot | July 19, 2022
https://www.inquirer.com/health/philadelphia-monkeypox-vaccine-virus-outbreak-20220719.html - Exposed to mpox? Here’s how to get a vaccination appointment in Philly | July 19, 2022
https://www.inquirer.com/health/monkeypox-vaccine-philadelphia-jynneos-20220719.html - Pa. got more than 3,000 doses of monkeypox vaccine this week, but access is still limited | July 15, 2022
https://www.inquirer.com/health/monkeypox-vaccine-philadelphia-rising-cases-pennsylvania-20220715.html - Mpox vaccines coming to Philly, but health officials say it’s not enough | July 9, 2022
https://www.inquirer.com/news/monkeypox-virus-disease-outbreak-philadelphia-cases-20220708.html

